The vast majority of newborns require no intervention at birth other than routine normal care. If this is done well, it vastly reduces the likelihood of problems. Most newborns should be transferred to the post-natal wards for rooming-in with their mothers. These babies still need to be monitored because they are at continued risk of hypothermia and feeding difficulties during the first few days of life. These babies can also become sick and develop danger signs. The mother needs counselling and appropriate treatment when required. Babies born in health facilities should not be sent home in the crucial first 48 hours of life. Follow-up care should be organised before the mothers are discharged (also see the chapter on discharge from the hospital. Take time to counsel her and involve another guardian, where possible. Ensure that they understand the implications of leaving early, advise them on danger signs, and arrange a follow-up plan for the baby.
A post-natal room should be kept warm with no draughts from open doors or windows. A room temperature of at least 25oC is required to help keep the baby warm. A mother and her baby should be kept together from birth if possible. This helps the mother form an early, close-loving relationship (bonding) with her baby. She can also respond quickly when her baby wants to feed, which helps establish breastfeeding and reduces breastfeeding difficulties (1).
Review the labour and birth record to identify risk factors or any events during the birth that may be important in the management of the mother and the baby.
| Key Facts for Providers: Routine Care of the Term Newborn | |
|
|
Examine the baby according to the postnatal ward policy, but at least twice a day for the first 48 hrs.
| Key Facts for Providers:
How to Examine the Newborn |
|
|
On admission (day zero) to the post-natal ward, at 24 hours, and at discharge check:
|
|
Signs should be assessed during each post-natal care contact, and the newborn should be referred for further evaluation if any danger symptoms or signs are present (see “Danger Symptoms or Signs for list).
| Key Facts for Providers: Danger Symtoms or Signs | |
|
|
At each post-natal contact, parents should be offered information and guidance to enable them to care for their baby.
| Key Facts for Providers and Mothers/Guardians | |
| Warmth | Appropriate clothing of the baby for ambient temperature is recommended. This means 1-2 layers of clothes more than adults and use of hats/caps. |
|---|---|
| Skin | Babies are not bathed routinely in the hospital so as to prevent complications like hypothermia and infection. They may however be sponged with lukewarm water. |
| Cord Care | Chlorhexidine is applied once after birth. After this, instruct the mothers not to apply anything to the cord but keep it clean and dry and outside the nappy. Note: do not apply spirit or salty water. |
| Nappy Rash | Nappy rash is worse when plastic pants are used and retain urine on the skin. Prevent with frequent nappy changes, cleansing, and exposure of the perineal area in order to reduce baby’s contact with faeces and urine. Cleansing agents should not be added to bath water nor should lotions, powder, or medicated wipes be used. When required, the only cleansing agent that should be used is mild non-perfumed soap. |
| Thrush | If thrush is identified in her baby, the woman should be offered information and guidance about relevant hygiene practices i.e., hand washing with soap, clean bra. Symptomatic thrush (difficulty feeding) requires antifungal treatment. |
| Jaundice | Parents should be offered information about jaundice including that: 50% of newborns and 80% of preterm babies have some jaundice. It may be normal or abnormal. Normal or physiological jaundice occurs around 3-4 days after birth. The mother of a breastfed baby who has signs of jaundice should be actively encouraged to breastfeed frequently, and the baby awakened to feed, if necessary. Breastfed babies with jaundice should not be routinely supplemented with formula, water, or dextrose water. Parents should be advised to contact the health facility if their baby’s jaundice is worsening, or if their baby appears unwell in any way. If jaundice remains after 14 days in an otherwise healthy baby (21 days in preterm babies), it should be evaluated. |
| Weight Loss | Weight loss of up to 10% in the first days of life is normal. Most term infants regain their birth weight by 10-14 days |
| Hygiene | Advise the mother to wash her hands with soap and water before and after using the toilet and before and after cleaning the baby. |
| Danger Signs | Remind the mother about danger signs and care seeking. |
| Transitional Stools |
The passage of frequent, loose stools, yellowish-greenish in colour between days 3 and 14 of life is normal and needs no treatment. |
| Vaginal White Discharge/ Bleeding |
This is normal. |
Benefits of Breastfeeding
Babies who are exclusively breastfed for six months will get the greatest health benefits and
disease prevention.
Colostrum (first yellowish milk after delivery) – this will meet the needs of the baby in the first few days after birth.
Discomfort for the mother at the start of breastfeeds in the first few days is not uncommon, but this should not persist. Benefits of breastfeeding to the mother include:A baby may have a variable feeding pattern, at least over the first few days, as the baby takes small amounts of colostrum and then takes increasingly larger feeds, as mother’s milk supply comes in. When the milk supply is established, a baby will generally feed every 2–3 hours, but this will vary between babies and, if the baby is healthy, his/her individual pattern should be respected. Empty both breasts at each feed.
Ask mother if the infant has breastfed in the previous hour.
If infant has not fed in the previous hour, ask why so that you can understand if there are any
challenges or misunderstandings. Regardless of the reasons given, ask the mother to put her
infant to the breast and assess for the following:
Observe the breastfeed. Signs of good positioning:
Signs of good attachment:
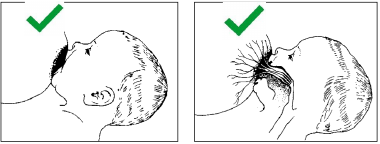
Bad attachment:
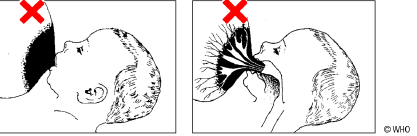
Poor attachment results in painful nipples → breast milk is not removed effectively thus causing breast engorgement → poor milk supply, hence baby is not satisfied and irritable → breast produces less milk, resulting in a frustrated baby who refuses to suck → poor weight gain.
3. SuckingEffective sucking occurs when the infant makes slow deep sucks, sometimes pausing. If not sucking well, then look for ulcers or white patches in the mouth (oral thrush).
| Key Facts for Providers and Mothers/Guardians: Breastfeeding | |
If breastfeeding is not progressing, support and assistance with positioning and attachment on the breast should be provided. If nipple pain persists after repositioning, consider evaluation for thrush or cracks. If signs and symptoms of engorgement are present, the mother should be encouraged to:
If signs and symptoms of mastitis are present (red, tender, hot segment or whole breast, mother may be febrile), a woman should be advised to do the following:
|
|
If signs and symptoms of mastitis persist more than several hours, the mother should contact her healthcare provider and may require antibiotic treatment. If the baby is not taking sufficient milk directly from the breast and supplementary feeds are necessary, expressed breast milk should be given by a cup or spoon; supplementation is not recommended.
All babies born to HIV positive mothers should be managed according to the current Malawi Integrated Guidelines for providing HIV services in Children and Adults (2). The lactating mother should be treated with antiretroviral (ARV) medication.
Nevirapine syrup is given to all HIV exposed babies as soon as possible after birth until six weeks of age.
| Birth Weight | Dose of Nevirapine |
|---|---|
| <2500g | 1.0 ml P.O. every 24 hours |
| >2500g | 1.5 mls P.O. every 24 hours |
At six weeks, the following is required:
Test the mother for syphilis if she was not been tested in the last three months. Treat all infants of mothers who are VDRL seropositive and are untreated or inadequately treated or if there is no clear documentation of full treatment. Check if the partner was treated as well. If unsure, it is safer to treat. Please note that there may be no clinical signs of infection or a variable number of signs.
| Clinical Findings Suggestive of Syphilis |
Treatment |
|---|---|
|
|
If the mother has active lung tuberculosis (TB) in the third trimester or TB was diagnosed after delivery, manage according to the National TB Control Programme guidelines. Examine her baby closely for symptoms and signs of disease. If the baby is well, commence isoniazid (H) prophylaxis at 10 mg/kg/day and do not give BCG vaccine.
Re-evaluate the infant at the age of six weeks, noting weight gain, and taking an X-ray of the chest, if possible. If the infant is doing well and tests are negative, continue prophylactic isoniazid to complete six months of treatment.
If any findings suggest active disease, start full anti-TB treatment, according to national guidelines.
Dose of Isoniazid (H) for NYI Exposed to TB but Not Infected
| Baby’s Weight | Isoniazid Dose |
|---|---|
| <2500g | 25mg (1/4 tablet) every 24 hours |
| 2500-5000g | 50mg (1/2 tablet) every 24 hours |
If the baby is not well at birth and has signs/symptoms suggestive of TB disease, collect gastric aspirates first thing in the morning using a nasogastric tube. Send for Gene X-pert and culture where possible, and commence full TB treatment according to national guidelines. Be aware that the absence of TB in gastric aspirate does not exclude TB and the whole clinical picture must be taken into account.
Correct planning of discharge from the hospital is very important for the newborn.
Infants who are discharged from the hospital should return for follow-up care to the nearest health facility at one week and six weeks. If any danger sign is present, the baby should be brought to the clinic immediately. Communicate with the health personnel who will be responsible for follo-up care by writing in the health passport.
Also see the chapter on discharge for more information
| Key Facts for Providers and Mothers/Guardians: Discharge |
|